(Ars Technica, June 16, 2020):
“Mutation may be helping the coronavirus spread more readily -
A mutation that’s becoming common seems to boost infectivity in cultured cells.”
.
(Scripps Research Institute, June 12, 2020):
“Mutated coronavirus shows significant boost in infectivity -
COVID-19-causing viral variant taking over in the United States and Europe
now carries more functional, cell-binding spikes.”
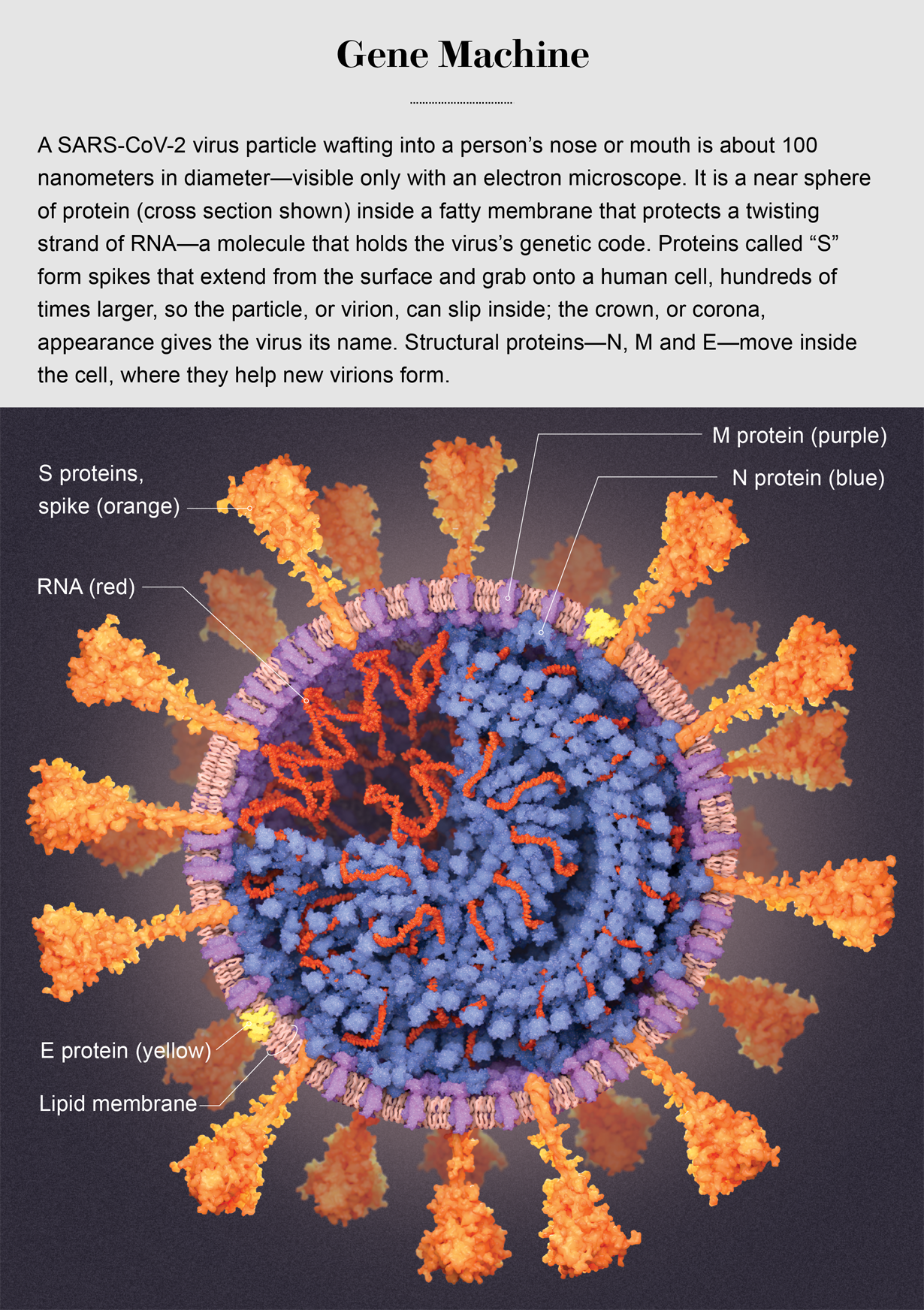
A tiny genetic mutation in the SARS coronavirus 2 variant circulating throughout Europe and the United States significantly increases the virus’ ability to infect cells, lab experiments performed at Scripps Research show.
“Viruses with this mutation were much more infectious than those without the mutation in the cell culture system we used,” says Scripps Research virologist Hyeryun Choe, PhD, senior author of the study. The mutation had the effect of markedly increasing the number of functional spikes on the viral surface, she adds. Those spikes are what allow the virus to bind to and infect cells. “The number - or density - of functional spikes on the virus is 4 or 5 times greater due to this mutation,” Choe says.
The spikes give the coronavirus its crown-like appearance and enable it to latch onto target cell receptors called ACE2. The mutation, called D614G, provides greater flexibility to the spike’s “backbone,” explains co-author Michael Farzan, PhD, co-chairman of the Scripps Research Department of Immunology and Microbiology. More flexible spikes allow newly made viral particles to navigate the journey from producer cell to target cell fully intact, with less tendency to fall apart prematurely, he explains. “Our data are very clear, the virus becomes much more stable with the mutation,” Choe says. …
… “There have been at least a dozen scientific papers talking about the predominance of this mutation,” Farzan says. “Are we just seeing a ‘founder effect?’ Our data nails it. It is not the founder effect.”
Choe and Farzan’s paper is titled “The D614G mutation in the SARS-CoV-2 spike protein reduces S1 shedding and increases infectivity.”
.
Some earlier comments and papers regarding SARS-CoV-2 Mutation D614G:
(May 12, 2020):
“EXPERT COMMENTARY: ‘D614G’ mutation of SARS-CoV-2,
the virus that causes COVID-19”
Two-thirds of the sequenced strains (or “isolates”) globally and half of the sequences in some countries (such as Australia and India) now have this D614G mutation, which is apparently increasing its representation among newer strains. … the D614G strain is only one of currently 10 strains circulating.
.
(AAAS, May 7, 2020):
“Mutations in the Coronavirus Spike Protein”
.
(May 5, 2020):
“Global Spread of SARS-CoV-2 Subtype with Spike Protein Mutation D614G
is Shaped by Human Genomic Variations that Regulate Expression
of TMPRSS2 and MX1 Genes”
SARS-CoV-2, particularly the 614G subtype, has spread more easily and with higher frequency to Europe and North America where the delC allele regulating expression of TMPRSS2 and MX1 host proteins is common, but not to East Asia where this allele is rare.